The Pink Journey Foundation
Our Optimal Screening Guidelines
Introduction:
There is general agreement that screening mammography saves lives. A recent study of nearly 550,000 women concluded that mammographic screening reduced breast cancer mortality rates by 41% (Ref. 1). Another recent report concluded that when breast cancers are detected on screening mammograms in women with no breast symptoms their chances for survival were 98%. (Ref. 2).
Despite the proven benefits of mammographic screening, a recent study from the National Cancer Institute (NCI) showed major challenges persist. The study by the NCI concluded that 20% of early-stage breast cancers are not detected on standard mammographic screening (Ref. 3).
Breast density:
The failure to detect small breast cancers on the screening mammogram is directly related to the issue of breast density (Breast Density). Seventy-four percent of women between ages 40 and 49 have dense breasts (Ref. 4). Dense breast tissue appears white on the mammogram and small breast cancers are also white. Finding small cancer in a dense breast has been compared to the challenge of finding a snowman in a snowstorm.
Thus, not only are breast cancers more difficult to detect in women with dense breasts, but breast density is a major risk factor for developing breast cancer (Ref. 5). A study from a major university concluded that “dense breasts eclipse all other known breast cancer risk factors” (Ref. 6).
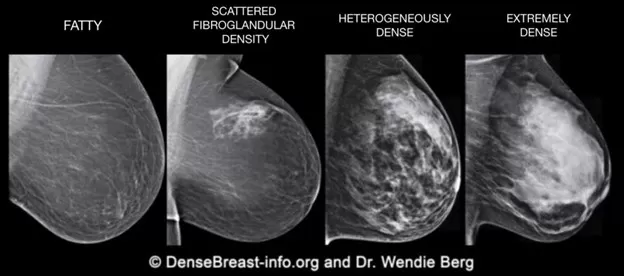
There are four patterns of breast density (Fig. 1). Fatty and scattered fibroglandular density are both considered to be fatty patterns. Heterogeneously dense and extremely dense are classified as dense breasts. The greater the level of breast density the higher risk for developing breast cancer.
Figure 1:
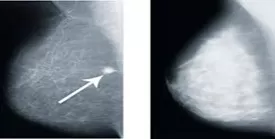
An example of the challenge of detecting small breast cancers in a woman with dense breasts is illustrated in Figures 2 and 3. Figure 2 shows a small white breast cancer in a woman who has a fatty breast pattern. Cancer is easily detected in a breast with fatty breasts (see arrow). Figure 3 is a mammogram of another woman who has a similar-sized breast, but it is extremely dense. The small breast cancer noted in fig. 2 could easily be obscured in fig. 3 by the surrounding tissue making it extremely difficult to visualize.
Figures 2 and 3:
New Technology:
Major advances have been made in screening technology. The 3-D screening mammogram (also referred to as tomosynthesis) is more effective in detecting small cancers than is the standard 2-D mammograms (Ref. 7). Average-risk women who are found to have dense breasts on screening mammograms benefit from having an additional yearly whole breast screening ultrasound (Ref. 8). Women who have a strong family history of breast cancer are advised to have a yearly MRI in addition to their mammogram (Ref. 9). We are convinced that women who take advantage of these new technologies will have a survival advantage compared to women who do not participate in aggressive screening.
Artificial Intelligence:
Another major advancement in breast imaging is the application of Artificial Intelligence (AI) to the screening process (Artificial Intelligence). The incorporation of AI into the screening process is an emerging field that is very promising in the early detection of breast cancer (Ref. 10). AI-assisted mammograms can detect small cancers that are missed on the standard mammogram. An early report on the value of AI concluded that 31% of cancers not seen on the standard mammogram could be detected on the AI-assisted mammogram (Ref. 4). A more recent study found that AI detected 79% (27 of 34 patients) of the cancers that were missed on the screening mammogram (Ref. 11). Another recent report noted that breast cancer was detected on the AI assisted mammogram 4 years before it was detected on the standard mammogram (Ref .12).
A second concern about standard screening mammography is the high rate of negative breast biopsies (referred to as false positive biopsies). AI-assisted mammograms can reduce the rate of unnecessary biopsies by 69% (Ref. 13). It has also been recently reported that AI-assisted ultrasound and AI-assisted MRI also reduce the rate of unnecessary breast biopsies (Ref. 14-15). Reducing the rate of unnecessary biopsies decreases both the emotional and financial costs of having unnecessary breast biopsies.
It is time to rethink screening guidelines:
Current guidelines on the age to start yearly screening are evolving. In the past, it was recommended that mammographic screening start at age 50 (Ref. 16). Until recently we recommended that women start yearly screening at age 40 (internal link 40 not 50). We are now convinced that more aggressive screening will save lives and reduce the long-term costs of breast cancer care (Cost & Benefits).
A recent review of over 5.7 million mammograms concluded that women with one of three major risk factors should start yearly mammographic screening at age 30 (Ref. 17-18). The three risk factors include 1. Breast density 2. Strong family history 3. A personal history of early-onset breast cancer. This study supports the concept that all women should be given the option of having a baseline mammogram at age 30. Women who have dense breasts or other major risk factors would be advised to continue yearly mammographic screening. Women whose breasts are not dense and who have no other risk factors would be given the option to delay yearly screening to age 40.
The rationale to start screening at age 30 is supported by the finding that women in their 30s are more likely to be diagnosed with high-grade fast-growing breast cancers than are women in their 40s (Ref. 19).
Radiation Concerns
Mammograms expose the breasts to small amounts of radiation. But the benefits of mammography outweigh any possible harm from the radiation exposure (Ref. 20). One recent study concluded that the radiation dose required to perform a mammogram is about the same as the amount of radiation a woman would get from her natural surroundings every seven weeks (Ref. 21)
One option for young women who are concerned about the radiation risk should consider the option to start yearly whole breast screening ultrasound at age 30 (Ref. 22). One recent study concluded that the ultrasound is more sensitive than the mammogram in detecting small breast cancers in young women with dense breasts (Ref. 23).
However, women who choose to substitute a screening ultrasound for a mammogram should be aware that the mammogram is more effective in detecting calcifications which may be the first indicator of non-invasive breast cancer (Ref. 24). Non-invasive breast cancer is also referred to as ductal carcinoma in-situ (DCIS) (Ref. 25).
Women at High Risk:
Young women with a strong family history of breast cancer or other major risk factors should be referred to a breast care center (Ref. 26). Women who are confirmed to be at high risk are advised to have a baseline MRI by the age of 30 or sooner in selected cases (Ref. 27).
A recent study concluded that very high-risk women such as women with a BRCA mutation should have a twice-yearly MRI. All the cancers detected in this study were either early-stage invasive cancer or DCIS (Ref. 28).
High-risk women are also advised to have a clinical breast examination twice yearly. We recommend that all women learn to do monthly breast self-examinations starting in their early 20s (Breast Self-Exam and video).
Cost As a Barrier to Screening:
Cost is a major barrier to starting screening before the age of 40. Insurance will usually cover the costs of screening if there is a strong family history of breast cancer or other risk factors. Women who do not have risk factors will usually be required to pay out of pocket. The average cost of a screening mammogram is in the range of 300 dollars. Help is available to assist uninsured or underinsured women to find a high-quality mammogram at a lower price (Link to underserved populations: Ref. 29-30).
We advise young women to consider the potential benefits of screening before concluding that it is too costly. The major benefit of screening is to detect early-stage breast cancers that are potentially curable. However, a second important benefit is giving a woman the peace of mind of knowing that she does not have detectable breast cancer. To put the cost in perspective, the cost of a screening mammogram is in the range of purchasing a daily cup of coffee for a year. Investing in early detection could prove to be the bargain of a lifetime.
Questions? Contact us.
References:
- Mammography screening reduces rates of advanced and fatal breast cancers: Results in 549,091 women.
https://pubmed.ncbi.nlm.nih.gov/32390151/
- Free Breast Cancer Screening & Prevention
https://www.webmd.com/health-insurance/free-breast-cancer-screening
- The relationship of mammographic density and age: implications for breast cancer screening.
https://pubmed.ncbi.nlm.nih.gov/22358028/
- Women with Dense Breasts Have Higher Risk of More Aggressive Cancer
https://www.breastcancer.org/research-news/20110801
- Dense Breasts’ Eclipse All Other Known Breast Cancer Risk Factors
https://www.ucsf.edu/news/2017/02/405711/dense-breasts-eclipse-all-other-known-breast-cancer-risk-factors
- 3-D Mammography More Likely to Find Small Invasive Breast Cancers, Especially in Women Younger Than 50
https://www.breastcancer.org/research-news/3d-mammos-more-likely-to-find-small-invasive-bc
- Screening breast ultrasound: past, present, and future
https://pubmed.ncbi.nlm.nih.gov/25615743/
- Breast MRI (Magnetic Resonance Imaging)
https://www.breastcancer.org/screening-testing/breast-mri
- Artificial Intelligence in Breast Cancer Screening and Diagnosis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9650950/
- Retrospective Review of Missed Cancer Detection and Its Mammography Findings with Artificial-Intelligence-Based, Computer-Aided Diagnosis
https://pubmed.ncbi.nlm.nih.gov/35204478/
- AI detecting breast cancer 4 years before it developed.
https://www.cnn.com/videos/health/2023/03/07/artificial-intelligence-breast-cancer-detection-mammogram-cnntm-vpx.cnn
- Reduction of False-Positive Markings on Mammograms: A Retrospective Comparison Study Using an Artificial Intelligence-Based CAD
https://pubmed.ncbi.nlm.nih.gov/30963339/
- Artificial intelligence system reduces false-positive findings in the interpretation of breast ultrasound exams
https://www.nature.com/articles/s41467-021-26023-2#:~:text
- Artificial Intelligence Applied to Breast MRI for Improved Diagnosis:
https://pubs.rsna.org/doi/full/10.1148/radiol.2020200292
- Breast Cancer: Screening
https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/breast-cancer-screening
- Some Women Should Begin Mammograms in Their 30s, Study Say
https://www.hackensackmeridianhealth.org/en/healthu/2018/12/21/some-women-should-begin-mammograms-in-30s#.ZA4Be-zMJmA15
- New study supports mammography screening at 30 for some women
https://www.sciencedaily.com/releases/2018/11/181128082724.htm
- Unique Issues for Young Women with Breast Cancer
https://www.komen.org/breast-cancer/treatment/by-diagnosis/young-women-and-breast-cancer
- Mammogram Basics
https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/mammograms/mammogram-basics.html
- How dangerous is radiation from a mammogram?
https://www.eehealth.org/blog/2018/04/radiation-from-a-mammogram/
- The Role of Ultrasound in Screening Dense Breasts—A Review of the Literature and Practical Solutions for Implementation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5872003/
- Comprehensive Comparison of Diagnostic Accuracy of Ultrasound and Mammography in Young Women with Radiographically Dense Breasts
https://www.fortunejournals.com/articles/comprehensive-comparison-of-diagnostic-accuracy-of-ultrasound-and-mammography.pdf
- Understanding Breast Calcifications
https://www.breastcancer.org/screening-testing/mammograms/what-mammograms-show/calcifications
- Ductal Carcinoma in Situ (DCIS) Program
https://www.dana-farber.org/ductal-carcinoma-in-situ-program
- High Risk Breast Clinic
https://www.uclahealth.org/medical-services/cancer-services/breast-cancer/breast-health-services/high-risk-breast-clinic
- Effectiveness of MRI in screening women for breast cancer: a systematic review
https://www.futuremedicine.com/doi/10.2217/bmt-2021-0016
- MRI Twice per Year May Be Better Than Annual Mammogram for Finding Early Breast Cancers in High-Risk Women
https://www.breastcancer.org/research-news/mri-twice-a-year-better-than-annual-mammo
- Where to Get a Mammogram
https://www.breastcancer.org/screening-testing/mammograms/where-to-get-mammogram
- Susan G. Komen Breast Care Helpline
https://www.komen.org/support-resources/breast-cancer-helpline/